- Raising Brilliance
- Posts
- Why Autism and Celiac Disease Often Go Hand-in-Hand
Why Autism and Celiac Disease Often Go Hand-in-Hand
Learn why autism and celiac disease often go hand-in-hand, how to spot symptoms, and get expert tips for families managing both conditions.
Understanding the Autism-Celiac Connection: What Parents Need to Know

Autism and celiac disease appear together more often than chance would suggest, leaving many parents wondering if there's a real connection between these two conditions.
Quick Answer: Research shows children with autism may have celiac disease at rates 2-20 times higher than typical children, though studies vary widely. While most children with autism don't have celiac disease, the overlap is significant enough that experts recommend testing when gastrointestinal symptoms are present.
Key Facts | What This Means |
|---|---|
Autism affects 1 in 36 children | Very common developmental condition |
Celiac disease affects ~1% of children | Less common but often undiagnosed |
Up to 70% of autistic children have GI symptoms | Digestive issues are frequent in autism |
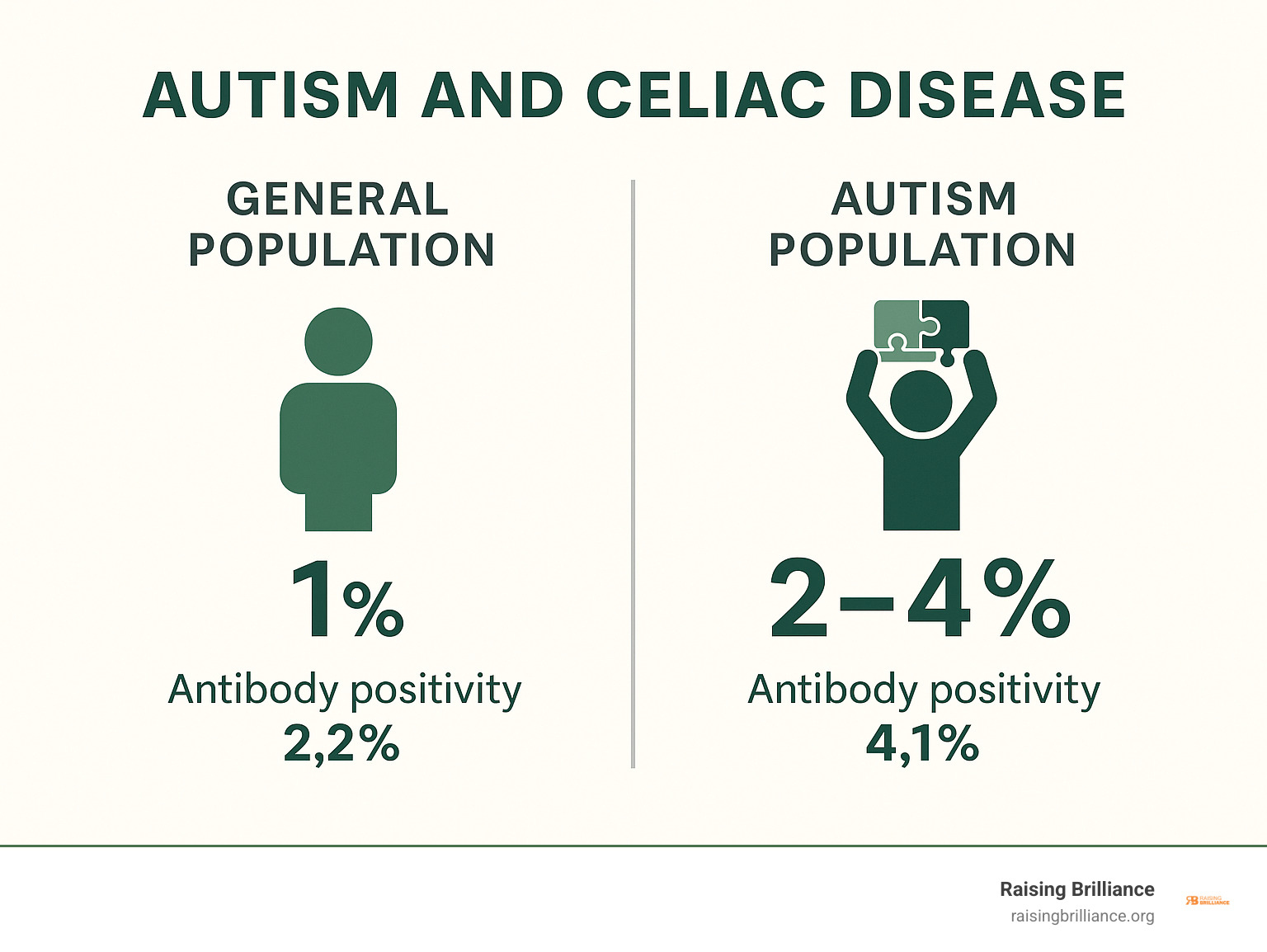
2-4% of autistic children may have celiac disease | Higher than general population |
If your child has autism and struggles with stomach pain, diarrhea, constipation, or poor growth, they might benefit from celiac disease testing. The good news? Both conditions are manageable when properly identified and treated.
The connection likely involves the gut-brain axis - the complex communication network between our digestive system and brain. When the gut is inflamed (as in celiac disease), it can affect brain function and behavior.
This doesn't mean every autistic child needs a gluten-free diet. But understanding when testing makes sense can help you make informed decisions for your family.

What Exactly Is Celiac Disease?
Think of celiac disease as your body's immune system getting confused and attacking itself. When someone with celiac disease eats gluten - that protein hiding in wheat, rye, and barley - their immune system mistakenly thinks it's under attack.
Here's what happens: The body creates antibodies to fight this perceived threat, but these antibodies end up damaging the tiny finger-like projections called villi that line the small intestine. These villi are incredibly important because they're responsible for absorbing all the nutrients from food.
When the villi get damaged (doctors call this villous atrophy), your child's body can't properly absorb vitamins, minerals, and other essential nutrients. Over time, this can lead to malnutrition, anemia, bone problems, and other health issues.
What makes celiac disease so tricky for parents is that symptoms can look completely different from one child to another. Some kids have obvious digestive problems, while others might just seem tired or have trouble growing properly.
The diagnosis process involves looking for several key markers. Tissue transglutaminase antibodies (tTG-IgA) serve as the most common screening test - think of these as red flags your immune system waves when it encounters gluten. Endomysial antibodies (EMA) are another type of antibody that's highly specific for celiac disease.
Doctors also check for genetic markers called HLA-DQ2 and HLA-DQ8, which are present in about 95% of people with celiac disease. If your child doesn't have these genes, celiac disease is extremely unlikely. Finally, an intestinal biopsy shows the actual damage patterns, which doctors grade using the Marsh classification system.
Test Type | What It Measures | When It's Used |
|---|---|---|
Blood serology | Antibodies (tTG-IgA, EMA) | First screening step |
Genetic testing | HLA-DQ2/DQ8 genes | Rule out celiac disease |
Intestinal biopsy | Villous damage (Marsh grading) | Confirm diagnosis |
Scientific research on celiac guidelines emphasizes how important it is to follow proper testing protocols, especially in children where symptoms might be subtle or look like other conditions entirely.
How Celiac Disease Is Diagnosed in Children
Getting a celiac diagnosis for your child involves following specific steps that pediatric specialists have carefully developed. The European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) has created guidelines that most doctors follow worldwide.
The process starts with initial blood work while your child is still eating gluten regularly. This is crucial - if your child has already gone gluten-free, the tests might not show accurate results.
If those blood tests come back positive, your doctor will likely refer you to a pediatric gastroenterology specialist. These are doctors who focus specifically on digestive problems in children and have extra training in conditions like autism and celiac disease.
Most children will need an endoscopy with biopsy to confirm the diagnosis. During this procedure, the doctor uses a thin, flexible tube with a camera to look inside the small intestine and take tiny tissue samples. The ESPGHAN criteria help doctors determine when this step is necessary and when blood tests alone might be enough.
Genetic testing plays an important role too, especially when other tests are unclear. If your child doesn't have the celiac genes, doctors can confidently rule out the condition and look for other causes of their symptoms.
The most important thing to remember? Keep your child eating gluten until all testing is complete. Going gluten-free too early can make getting an accurate diagnosis much more difficult.
Autism Spectrum Disorder 101: Beyond Behaviour
When most people think about autism, they picture the behaviors they can see - a child who lines up toys, avoids eye contact, or has trouble with conversation. But autism spectrum disorder affects far more than just social communication and behavior patterns.
Autism influences how the entire body functions, including systems we don't often think about. The digestive system, immune system, and even sensory processing all work differently in many children on the spectrum. Understanding this bigger picture is especially important when we're exploring connections like autism and celiac disease.
Social communication challenges and restricted interests are certainly core features of autism. Your child might struggle with back-and-forth conversation, have intense fascination with specific topics, or engage in repetitive movements. But there's so much more happening beneath the surface.
Many children with autism experience sensory processing differences that affect how they interpret touch, sound, taste, and other sensations. This can make trying new foods incredibly challenging - and it might mask underlying digestive issues that would be easier to spot in other children.
Perhaps most relevant to our discussion is how autism affects the body's internal systems. Research shows that immune dysregulation is common in autism, with many children showing altered immune responses and increased inflammation. Their neurodevelopment continues to be shaped by these ongoing biological processes throughout childhood.

Common Gastrointestinal Complaints in Kids with Autism
If your child has autism, there's a good chance they've dealt with tummy troubles. Studies show that between 22.7% and 70% of children with autism experience digestive issues - a much higher rate than we see in typical children.
Constipation tops the list of complaints. Many parents find themselves dealing with this on a regular basis, sometimes severe enough to require medical intervention. On the flip side, diarrhea or loose stools can be just as problematic, and some children alternate between the two.
Abdominal pain presents a unique challenge in autism. Your child might not be able to tell you their stomach hurts. Instead, you might notice increased irritability, sleep problems, or more repetitive behaviors. These behavioral changes could actually be your child's way of communicating physical discomfort.
Food selectivity goes beyond typical autism preferences when poor appetite becomes a factor. While many children with autism have strong food preferences, underlying digestive issues can make this even more complicated. Some children develop an instinctive avoidance of foods that make them feel worse.
The root of many these problems may lie in dysbiosis - an imbalance in the gut microbiome. The collection of bacteria and other microorganisms living in the digestive tract appears different in many children with autism. This imbalance can contribute to digestive symptoms and may even influence brain function.
Intestinal permeability, sometimes called "leaky gut," is another piece of the puzzle. When the intestinal lining becomes more permeable than it should be, it can allow substances to cross into the bloodstream that normally wouldn't, potentially triggering immune responses and inflammation.
Do Autism and Celiac Disease Overlap?
Here's where things get really interesting for families dealing with both conditions. The question of whether autism and celiac disease actually occur together more often than we'd expect by chance has kept researchers busy for years.
The short answer? It's complicated, but there does seem to be a real connection - just not as dramatic as some early studies suggested.
When Italian researchers studied 223 children with autism, they found something fascinating. While 2.24% had full celiac disease (compared to 1.58% in typical kids), what really stood out was the antibody testing. A whopping 4.08% of autistic children had celiac antibodies in their blood, compared to just 2.22% of neurotypical children.
This tells us something important: even when children with autism don't have full-blown celiac disease, their immune systems are reacting to gluten at higher rates. Think of it like their bodies are raising a yellow flag about gluten, even if they haven't reached the red flag of celiac disease.
The research journey has been a bit of a rollercoaster. Early studies got everyone excited with claims that celiac disease was 20 times more common in autism. But as larger, more careful studies rolled in, the numbers became more modest - though still meaningful.
Is There More Celiac Disease in Autism?
The data varies quite a bit depending on which study you're reading, but here's what the research landscape looks like:
Small early studies painted a dramatic picture with sky-high rates of celiac disease in autism. Larger population studies brought us back down to earth, showing more realistic increases of about 2-3 times the normal rate. The most rigorous recent studies consistently find celiac disease in about 2-4% of children with autism, compared to roughly 1% in the general population.
A major systematic review looked at all the available studies and found something telling. While many individual studies showed no clear link, the handful of really high-quality, population-based studies did suggest a genuine association.
The challenge is that studying this connection is tricky. Many studies had small groups of kids, used different ways of diagnosing celiac disease, or had other issues that make it hard to draw firm conclusions.
But here's what we can say with confidence: the presence of celiac antibodies appears consistently higher in children with autism, even when they don't meet the full criteria for celiac disease. This suggests their immune systems are more likely to react to gluten, which could be contributing to some of the gut symptoms so common in autism.
Is There More Autism in Celiac Disease?
Flipping the question around - do people with celiac disease have higher rates of autism? - gives us even fewer studies to work with, but the findings are still intriguing.
A large Swedish registry study (the kind researchers love because it includes huge numbers of people) found no increased risk of autism diagnosis after someone was diagnosed with celiac disease. So having celiac disease doesn't seem to increase your chances of developing autism.
But here's where it gets interesting: mothers with celiac disease had three times the normal risk of having a child with autism. This suggests the connection might start even before birth, possibly involving antibodies crossing the placenta during pregnancy and affecting how the baby's brain develops.
This maternal connection opens up fascinating questions about how autoimmune conditions during pregnancy might influence neurodevelopment. It's still early research, but it gives us important clues about the complex relationship between immune function and brain development.
How the Gut–Brain Connection Might Tie Them Together
The gut-brain axis represents one of the most fascinating areas of modern medicine. This bidirectional communication network connects our digestive system with our central nervous system through multiple pathways:
The vagus nerve - directly connecting gut and brain
Immune signaling - inflammatory molecules affecting brain function
Microbial metabolites - compounds produced by gut bacteria that influence mood and behavior
Hormonal pathways - gut hormones affecting brain chemistry
Scientific research on gut microbiome shows that disruptions in gut health can lead to changes in brain function, behavior, and even development.
In celiac disease, gluten triggers intestinal inflammation and increases intestinal permeability (sometimes called "leaky gut"). This allows inflammatory molecules and partially digested proteins to enter the bloodstream, potentially reaching the brain and affecting its function.
For children with autism, who may already have differences in immune function and gut microbiome composition, this inflammatory cascade could be particularly problematic.
Gluten Sensitivity Without Celiac: What We Know
Not everyone who reacts to gluten has celiac disease. Non-celiac gluten sensitivity is a poorly understood condition where people experience symptoms when eating gluten but don't have the intestinal damage characteristic of celiac disease.
Research from Columbia University found that children with autism had significantly higher levels of IgG antibodies to gliadin (a component of gluten) compared to typical children. Importantly, these children didn't have the genetic markers or tissue damage associated with celiac disease.
This suggests that some children with autism may have an immune response to gluten that operates through different pathways than classic celiac disease. While we don't fully understand what this means clinically, it provides a potential explanation for why some families report improvements when their autistic children avoid gluten.
Managing Gluten and GI Symptoms: Practical Advice for Families
When you're wondering whether your child with autism might have celiac disease, it's natural to want answers quickly. But here's something crucial: don't start a gluten-free diet before proper testing. Going gluten-free too early can make accurate diagnosis nearly impossible, leaving you with more questions than answers.
The key is taking a methodical approach that puts your child's health first. Start by documenting what you're seeing - keep a detailed log of digestive issues, behavioral changes, and any patterns you notice. These details can be incredibly valuable for your healthcare team.
Next, have an honest conversation with your pediatrician about whether celiac testing makes sense for your child. They'll consider your child's symptoms, growth patterns, and overall health picture. If testing is recommended, it typically involves blood work first, and possibly an endoscopy if results suggest celiac disease.

If your child does have celiac disease, a strict gluten-free diet becomes essential - not optional. This means reading every label, checking with restaurants, and being vigilant about cross-contamination. It sounds overwhelming, but thousands of families manage this successfully every day.
Even if testing comes back negative but you still want to try eliminating gluten, work with a registered dietitian who understands both autism and celiac disease. Children with autism often have limited food preferences already, and removing gluten without proper planning can lead to nutritional gaps.
The good news is that many naturally gluten-free foods are often well-accepted by children. Rice and rice-based products tend to be crowd-pleasers, along with potatoes and sweet potatoes. Corn and corn-based products offer familiar textures, while plain meats, fish, eggs, and dairy products provide essential proteins. Fruits and vegetables remain naturally safe choices, and nuts and seeds can work well for children without allergies.
For families managing a gluten-free diet, staying on track can be challenging. Tools like the GlutenDetect Gluten Exposure Test Kit can help you monitor whether gluten is accidentally sneaking into your child's diet, giving you peace of mind about dietary compliance.
Should Every Child with Autism Be Tested for Celiac Disease?
Here's the straightforward answer: current medical guidelines don't recommend routine celiac screening for all children with autism. But that doesn't mean testing is never appropriate - it's all about recognizing when it makes sense.
Testing should be strongly considered when your child has persistent digestive symptoms like ongoing diarrhea, chronic constipation, or frequent abdominal pain. Poor growth or unexplained weight loss are also red flags that warrant investigation. If there's a family history of celiac disease or other autoimmune conditions, the risk increases significantly.
Sometimes the signs are more subtle. Behavioral changes that seem to coincide with eating patterns might be your child's way of communicating discomfort they can't express in words. Nutritional deficiencies - particularly iron, B vitamins, or vitamin D - can also signal absorption problems that celiac disease might cause.
The research backs up this targeted approach. That Italian study we mentioned earlier concluded that blanket screening isn't necessary beyond general pediatric recommendations, but symptomatic children absolutely should be evaluated.
Does a Gluten-Free Diet Improve Autism Symptoms?
This is probably the question you're most curious about, and honestly, the answer is more complex than we'd all like it to be. The scientific evidence for gluten-free diets improving core autism symptoms is limited and mixed - but that doesn't tell the whole story.
Most well-designed studies have found minimal to no benefit from gluten-free, casein-free diets specifically for autism symptoms. But these studies often have significant limitations: small sample sizes, short timeframes, difficulty maintaining true dietary compliance, and challenges measuring behavioral changes objectively.
Here's what we do know with confidence: if a child has both autism and celiac disease, treating the celiac disease properly can lead to meaningful improvements. These include better digestive symptoms, improved nutritional status, increased overall comfort, and potentially some behavioral improvements related to feeling physically better.
There's also documented evidence of children whose autism-like symptoms improved dramatically after celiac disease diagnosis and treatment. This suggests that in some cases, nutritional deficiencies from undiagnosed celiac disease can actually mimic or worsen autism symptoms.
The connection between autism and celiac disease may be more about overall health and comfort than about "curing" autism. When a child feels better physically - when their stomach doesn't hurt, when they're absorbing nutrients properly, when inflammation decreases - their ability to learn, communicate, and engage with the world often improves too.
Set realistic expectations if you decide to try a gluten-free diet. Look for improvements in digestive symptoms, sleep patterns, and overall comfort rather than dramatic changes in core autism characteristics. And remember - any dietary changes should be made with professional guidance to ensure your child's nutritional needs are fully met.
Frequently Asked Questions about Autism and Celiac Disease
Parents often have pressing questions when they're trying to understand the connection between autism and celiac disease. Here are the answers to the most common concerns we hear from families.
Can celiac disease present solely with behavioural symptoms?
This is one of the trickiest aspects of celiac disease - it can absolutely show up as behavioral changes without any obvious stomach problems. Your child might become more irritable, have trouble focusing, or experience mood swings that seem to come out of nowhere.
Silent celiac disease is more common than many people realize. Some children develop what looks like attention problems, anxiety, or even depression as their primary symptoms. The nutritional deficiencies from damaged intestines can affect brain function in subtle but important ways.
However, here's the catch - when doctors look carefully, there are usually some physical signs present. These might be things you wouldn't immediately connect to celiac disease, like being shorter than expected, having dental problems, or getting frequent headaches.
If your child with autism has unexplained behavioral changes, especially if they coincide with meal times or seem to come and go in patterns, it's worth discussing celiac testing with your pediatrician.
How long does it take for gut healing after going gluten-free?
The healing process happens in stages, and children typically bounce back faster than adults. Within the first few weeks, many families notice improvements in digestive symptoms like stomach pain or diarrhea. Your child might seem more comfortable and less irritable.
Full intestinal healing is a much longer process. The damaged villi in the small intestine need time to regenerate completely. For children, this usually takes 6 to 24 months of strict gluten-free eating. Adults can take even longer.
Your doctor will monitor progress through follow-up blood tests to check antibody levels. Sometimes they'll recommend a repeat endoscopy after a year or two to confirm that the intestines have healed properly.
The good news? Most children feel significantly better long before their intestines are completely healed. Many parents report positive changes within the first month of going gluten-free.
Are there reliable home tests for gluten exposure?
This is where we need to be really clear about what different tests can and cannot do. Home antibody tests that claim to diagnose celiac disease are not reliable and shouldn't be used for diagnosis. These tests often give false results and can lead families down the wrong path.
However, if your child already has a celiac disease diagnosis and is following a gluten-free diet, there are useful monitoring tools available. Urine tests that detect gluten peptides can help you figure out if your child has been accidentally exposed to gluten.
These tests, like the GlutenDetect kit, work by finding actual gluten proteins in urine within 6 to 24 hours of exposure. This can be incredibly helpful for families trying to identify hidden sources of gluten or confirm that symptoms are related to accidental gluten intake.
These monitoring tests only work for people who are already diagnosed and supposed to be gluten-free. They're not diagnostic tools - they're detective tools for families managing celiac disease day to day.
Conclusion
The relationship between autism and celiac disease is like many things in autism - more nuanced than we'd like, but important enough to understand. While most children with autism won't have celiac disease, the connection is real and worth paying attention to, especially when your child is dealing with tummy troubles.
Here's what really matters for your family: testing makes sense when you're seeing digestive symptoms, growth concerns, or there's a family history of autoimmune conditions. But here's the relief - most children with autism don't need gluten-free diets unless they actually have celiac disease. No need to stress about eliminating gluten "just in case."
The encouraging news is that both conditions are completely manageable when properly identified and treated. And while the science behind the gut-brain connection is still unfolding, it gives us a logical framework for understanding why these conditions sometimes show up together in the same child.
At Raising Brilliance, we get it - you're already juggling so many decisions and concerns as an autism parent. The last thing you need is another complicated medical puzzle to solve. While researchers continue studying the autism and celiac disease connection, what truly matters is finding the right path for your unique child.
If digestive issues are making life harder for your family, that conversation with your pediatrician is a great first step. Proper testing can give you real answers instead of guesswork. And if celiac disease is part of your child's story, treatment can make a genuine difference in their comfort and quality of life.
You're not navigating this journey alone. Our free autism resources include practical guides for managing medical concerns, working effectively with healthcare providers, and supporting your child's overall health and development - because every piece of your child's wellness puzzle matters.
Raising a child with autism means making countless complex decisions, but armed with good information and the right professional support, you can make choices that truly serve your child's best interests. Trust your instincts, ask good questions, and know that you're doing an amazing job.